Background
Maternal Mortality Ratio
One of the main indicators of the health status of a country is the Maternal Mortality Ratio (MMR). The MMR is the number of women who die from the beginning of a pregnancy until six weeks after delivery per 100,000 deliveries. The MMR shows the ability and the quality of health services, health services capacity, the quality of education and knowledge in a society, its health and environmental quality, and the availability of social and cultural information, as well as obstacles to gaining access to health services. A high MMR and the slow decline in this rate shows that improvements to service in Maternal and Child Health (MCH) are urgently required in terms of both the range and quality of services (Manuaba, 2008).
A report published by the World Health Organization (WHO) in 2011 shows that the worldwide MMR stood at 287/100,000 live births (0.287%). In 2012 the MMR stood at 270/100,000 live births. The sub-Saharan region of Africa and South Asia were the regions where the most deaths occurred. One-third of all maternal deaths in the year 2011 occurred in just two countries – namely India and Nigeria (Desita, 2012).
A high number of cases of maternal morbidity and mortality in many countries are due to postpartum hemorrhage, eclampsia, and complications of miscarriage. Most of the major causes of maternal deaths could be prevented. Through effective prevention, some developing countries and almost all developed countries managed to reduce maternal morbidity and mortality to very low levels (Utomo, 2007). The MMR in Indonesia in 2012 was 359/100,000 live births, an increase of approximately 57% compared to 2007, when it was 228/100,000 live births. The target Millennium Development Goals (MDGs), in which the government sought to reduce the MMR to 102/100,000 live births had not been achieved by 2015 (Ministry of Health, 2014).
PHC PONED in Indonesia
The Ministry of Health (MOH) continues to try to reduce the MMR and Infant Mortality Ratio (IMR) and high risks to pregnant women by improving the quality of services available to the community through efforts such as Primary Health Centers (PHC) capable of providing basic obstetric and neonatal emergency care, known as PONED (Desita, 2012). The cases handled in PHCs include bleeding during early pregnancy, postpartum hemorrhage, hypertension, prolonged labor, premature rupture of membranes, hypothermia, hypoglycemia, jaundice, seizures, and neonatal infections (Manuaba, 2008).
PHC PONED is a specialist medical service in PHCs meant to bring referral services to communities in need. This includes some emergency obstetric and neonatal care. The development, in practice, must consider a variety of requirements. PHC PONED centers have emergency service facilities for obstetric and neonatal care ready 24-hours/day to provide services for pregnant women, labor, delivery, and neonatal emergencies either in person or though referral, or through cadres (community members who trained to be secondary care providers in the community), village midwives, and PHCs (Prawirohardjo & Sarwono, 2004).
Previous research performed by Pattianakotta (2012), who researched PHCs in central Maluku, recommends having staff who have been trained in PONED, including doctors, midwives, and nurses. In addition, Desita (2012), who did research in PHCs in Tlogosari Kulon Karangmalang Semerang City, suggested that, in terms of PONED policy, the power should be with doctors, nurses, and midwives. According to Hasnah (2003), the role of implementing health services in PHCs with health workers is a strategic resource. Health workers were able to make optimal use of physical, financial, and human resources to help the team.
Baso PHC
The Maternal and Child Health Revolution Program (MCH Revolution) in Agam Regency was established through legislation to benefit mothers and children. MCH Revolution is one of the efforts to accelerate the reduction in maternal and neonatal mortality at adequate health facilities (Agam Health Departement, 2013). As a case study, we examine Baso PHC’s PONED services.
The PHC was created by the government through the MOH with the Regency Health Office to help accelerate the reduction of maternal and infant mortality because of a prior lack of commitment to PONED. To make a PHC capable of providing PONED services, various important preparation works was done, including preparation of buildings, equipment, personnel training, funding, and the preparation of the PHC administrators. All this preparation has been carried out by the Agam Regency Health Department to provide quality emergency services related to obstetric and neonatal care.
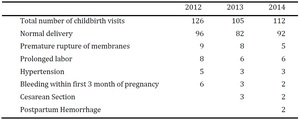
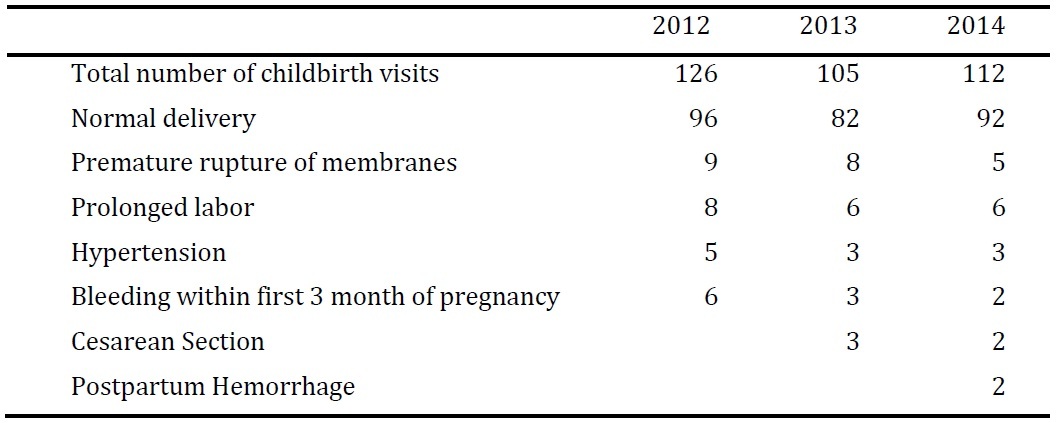
Baso PHC is one of the PHCs in the Agam Regency. Baso PHC was designated a PHC by the Regency Health Department in 2012. Between 2012 and 2014, a total of 343 women visited for childbirth-related reasons. Of those, 270, or approximately 79%, had normal deliveries. The remaining were referred to a hospital with a variety of conditions including premature rupture of membranes, prolonged labor, hypertension, bleeding within the first 3 months of pregnancy, having had a cesarean section with a previous birth, and postpartum hemorrhage.
Preliminary results of a study conducted in March 2015 are the basis for the following profile of Baso PHC health workers in 2014. The staff consists of as many as 12 people, including 8 midwives and 4 nurses. Of the 12 staff members at the Baso PHC, only one nurse has been trained by the Provincial Health Department. At this time, as described above, the only services provided in the PHC are normal delivery care. It seems that the PONED program has still not been fully implemented at the PHC in Baso, Agam Regency, Indonesia, because patients were still referred to a hospital for issues that are supposed to be able to be handled by a PHC PONED team.
Research Design
This study uses a qualitative approach. The aim of a qualitative research method is to gather greater in-depth information, to provide a greater understanding, and to get insight into the attitudes, beliefs, motivations, and behavior of respondents in regards to the implementation of PONED at Baso PHC. We applied a systems approach to offer suggestions to further improve the Baso PHC’s PONED services. The systems approach is the application of a systematic and logical way of thinking to discuss and find solutions to a problem or situation (Notoatmodjo, 2005).
The data for this study was collected from in-depth interviews. Respondents include the head of the Baso PHC, staff in charge of the PONED services, and community members who visited the Baso PHC for childbirth-related reasons while we were conducting our study. All the respondents were female, except for the head of the Baso PHC. The community members were all married women, 27-38 years old, and experiencing their first or second pregnancy. They had various levels of education, from a junior high school education through a university education.
Results
PHC PONED Planning and Resources
People involved in the planning and implementation of PONED include the head of the Provincial Health Department, the head of the Baso PHC, and other health organizations. Planning and implementation of the PONED process has a standard procedure, involving either the head of the PHC, the administrator of the PHC, or the PONED team. Planning is done by the leadership, administrator, and PONED team every year.
The planning standard of PONED consists of 3 parts: human resources, facilities, and infrastructure. Planning for human resources includes increasing the knowledge and ability of staff. Other considerations include the preparation of equipment, medicine, budgeting, and promotion.
The availability of resources to do PONED activities in the Baso PHC are still far from sufficient, as evidenced by information provided by participants. Of the 10 respondents, 7 of them said the Baso PHC lacked resources for each department to do PONED activities.
The staff of the Baso PHC also explained that training was only conducted in 2012, and only one staff member was trained. This confirms that training is not routinely done every year. All of the participants clarified the training was conducted a long time ago.
Seven respondents clarified that the facilities in the Baso PHC are insufficient to support PONED activities. The facilities, including the building, are only sufficient for general services.
Related to budgeting of PONED activities, 5 respondents declared the budgeting for PONED comes from the government budget, 2 of the respondents said the budgeting comes from the public health budget, and 3 others said they do not know where the budget comes from.
The methods which should be applied in the PONED implementation, as the respondents mentioned, include periodic supervision and evaluation of activities, a division PONED officer on call, and a refresher science training program each month, but there is no doctor on duty in this division, because there is no specialist PONED doctor in this PHC, only general doctors. No regular training has been provided, as mentioned above.
Operating Procedures
The process of PONED services in the Baso PHC was mentioned by 10 respondents. Of them, 4 said the PONED services are running smoothly, 5 others said PONED services are being done by the staff of the PHC but they did not know how smoothly it was running.
The formation of a PONED organization under the Province Health Department or the Regency Health Department, requires structural organization. Supervision of PONED services is conducted by the Regency Health Department and Provincial Health Department once every 6 months. There is documentation in the form of a monthly report on maternal and infant health outcomes. The report is given to the Regency Health Department office each month. Supervision of the centers has taken the form of regular monitoring conducted by the Provincial Health Department performed once in a 6-month period.
The obstacles encountered in the implementation of PONED in the Baso PHC are that resources, facilities, and infrastructure are insufficient, because too few staff members have trained for PONED, and the equipment and other facilities are not up to an appropriate standard yet. The community felt that the PONED program at the Baso PHC would be beneficial, even though it had not been implemented yet.
The staffing of the PHC is not yet sufficient, both in terms of the number of staff and the kind of staff available. There are 3 health professionals on a team, namely one doctor, one nurse, and one midwife, and the power structure is based on perceived competence, where the midwife specifically addresses labor, while doctors act as decision makers. The number of teams at this PHC is not sufficient. The qualifications of team members may also be insufficient. There are no special requirements to be on the team, because the team is appointed directly by the heads of PHCs. A team should not be moved to another PHC until 3 years after training.
Comparison to Other PHCs
My assumption is that the workforce for the PHC is inadequate because of their education and that many staff members who have received PONED training have moved. There should be 3 PONED teams so one is available every shift. In this case, training of future teams needs to be done regularly, in order to make the program sustainable.
In their activities, the PHC still has a PONED deficiency. The infrastructure is insufficient. In addition, PONED services are still unavailable, because PONED doctors can be redeployed to other PHCs.
The results of our study were similar to previous research performed by Desita (2012), which found that there are still various obstacles in terms of the implementation of PONED in Karang Malang Semarang.
The shortages that researchers have still been seeing were found to be true in the implementation of PHC PONED services in Baso. They were caused by facilities and infrastructure that are not up to appropriate standards and team personnel who could not handle emergency cases, causing a higher than desirable fraction of birthing mothers to be referred to a hospital. The absence of some team members during certain shifts was also problematic. The unavailability of special funds for operations also became an obstacle in the implementation of PONED services.
There is a lack of human resources in the Baso PHC so that gaps in the PONED system are still found. This can be improved gradually, and improvements of various deficiencies identified here can be used as evaluation criteria in the future.
Discussion
Preparation and Implementation
In order for a PHC to be able to run the PONED program optimally, one factor that should be considered is the preparation and implementation of PONED facilities and infrastructure, so they are equipped to handle labor cases well.
According to Hasnah (2003), physical resources are a means of supporting health workers so they can run an optimal health care facility. In accordance with previous studies there are constraints to program development, namely human resources, lack of infrastructure, and lack of decreed forms of financing or a letter of assignment, so that there is no clear legitimacy. The solution to development is the fulfillment of the agreement regarding infrastructure, training, and filing requirements by the government and sufficient financing to run it smoothly.
Based on the results of the in-depth interviews, we learned there are no funds specifically set aside for PONED activities. All support for PONED activities must come from the PHC budget, which must also support other programs at the PHC.
According to Wijaya (2012), sufficient preparation of a PONED-capable PHC is difficult if there are no funds and a lack of human resources and infrastructure. The allocation of special funds for the program is also an important factor. With the funds, the activities of PONED can be implemented because the PHC can procure the equipment and medication necessary for handling emergencies in labor.
When we began the research, we assumed the completeness of infrastructure and facilities, but the Baso PHC is still lacking both of these. However, PONED services have been implemented at a minimum standard and have been running smoothly for two years.
Additional funding is needed to ensure the completeness of infrastructure and facilities and to support staff in order to meet the expected standards. The goal is that eventually no cases that should be handled by the PHC will be referred to the hospital.
Implementation of PONED Services and Constraints Faced
The Baso PHC was founded 2 years ago. It still encounters some obstacles, such as a lack adequate training for staff, a lack of available funds from the government, and no specific allocation for funding PONED services. The low operational budget is used for the procurement of devices, medication, building repairs, and for staff.
The other problems are in terms of human resources, funding, and also implementation. PONED services in Baso PHC still have shortcomings in terms of publicization as a PONED PHC, so that there are still people who do not understand about the PHC. Public relations are very important, because all pregnant women should know about the program, so that they can understand and be aware of safety in the delivery process. According to a study by Ilyas et al. (2005), there are many obstacles encountered by citizens who know less about the dissemination of PONED services.
Based on the results of interviews that have been conducted, we found that efforts that should be made to overcome the problems in terms of the Baso PHC PONED implementation are as follows:
-
Draft a proposal to the Agam Regency Health Department asking for an increase in the PHC PONED budget.
-
Propose that the Provincial Health Department conduct additional team training.
-
Improve dissemination of information about PONED PHCs from the Provincial Health Department to midwives and community leaders.
-
Ensure there is a PONED team on duty each shift.
-
Foster a sense of commitment and consistency to the whole range of staff involved in the service implementation of PONED.
We assume that efforts made by the PHC in addressing the issue have been quite good, but 1 additional PONED team is not sufficient for 3 shifts. Therefore, additional teams are needed. For this, PHCs need support from community leaders like the village trustee, so that the whole community knows about PHC PONED. Input from the community should also be noted, including the attitude of the community towards the implementation of the program in the future.
Conclusion
Based on the research that has been conducted through in-depth interviews with various sources and also observation of obstetric and neonatal emergency care at the Baso PHC, Agam in 2015, we made the following conclusions: There was a lack of human resources for PONED services in terms of enough staff members with sufficient knowledge and skills, as well as insufficient facilities and infrastructure, causing many cases that should have been handled by the PONED team to be referred to the hospital. There are many obstacles encountered in the implementation of care in the Baso PHC.
Suggestions
Further planning should include an increase of trained personnel in PONED services. The staff on duty should be more active in conveying information to the public related to the benefits of PONED for the community. Suggestions should be forwarded to the management and the Regency Health Department to improve services as well as dedicated funding in each PHC. The government, especially the Agam Regency Health Department, should have policies to support the PHC PONED activities of the PHC. Improved facilities will improve the quality of PONED services. The PONED team should be able to provide emergency obstetric and neonatal services in a professional manner. Future research should be conducted to assess the implementation of the program.
Biographical Note
Dr. Evi Hasnita is the coordinator of AIPKIND (the Midwivery Educational Association) forWest Sumatra, Riau, Jambi, and Jambi Island Province, Indonesia and the director of STIKes Fort De Kock Bukittinggi in West Sumatra Indonesia. She earned her doctorate in public health from Gadjah Mada University.
She can be reached at STIKes Fort De Kock Bukittinggi, St. Soekarno Hatta, Manggis Gantiang, Mandiangin Koto Selayan, Bukittinggi, West Sumatra, Indonesia or by email at evi.hasnita@yahoo.co.id.
Correspondence
All correspondence concerning this article should be addressed to Evi Hasnita at STIKes Fort De Kock Bukittinggi, St. Soekarno Hatta, Manggis Gantiang, Mandiangin Koto Selayan, Bukittinggi, West Sumatra, Indonesia or by email at evi.hasnita@yahoo.co.id