Background
The ultimate goals of the dynamic changing healthcare system are to make it easier to access, improve people’s self-care, and to provide early detection of health problems, along with greater equity of healthcare services. Healthcare institutions differ in their capability in offering services depending on their resources, such as staffing, and the local environment (Surakka, 2008). Healthcare providers should also be competent in their roles. Nurse managers are positioned to be leaders and facilitators for clinical decision-making at the unit level (Cioffi & Ferguson Am, 2009). Moreover, nurse managers should create a safe unit, monitor quality care, demonstrate vision, manage the nursing flow, and maintain patient satisfaction (Eggenberger, 2012; Roussel & Swansburg, 2009). They need to relay policies from the directors of nursing to their staff, and work with their unit staff to achieve goals (Surakka, 2008). Therefore, they need to have specific skills to be competent in their positions. A critical review of the literature also revealed competence in nurse managers influences a healthy environment in workplace, staff and clients’ satisfaction, and quality healthcare (Aiken et al., 2011; Brady Germain & Cummings, 2010).
Many researchers have defined competency. Vazirani (2010) reviewed the literature and found that competencies are skills, knowledge, and the underlying characteristics of a person that demonstrate behavioral or thinking methods in a variety of situations. Spencer and Spencer (1993) identified five components of competency characteristics including knowledge, skills, motives, traits, and self-concept, which emphasize the point that competencies are associated with performance in the workplace.
In Thailand, healthcare services are divided into three levels of care including primary care, secondary care, and tertiary care. Secondary care is classified into several levels such as 1) a small community hospital which serves uncomplicated and low risk patients 2) a medium-sized community hospital which serves complicated patients 3) a large community hospital which serves patients with more complications than a medium level hospital. Community hospitals, the majority of hospitals in Thailand (72%), are classified as secondary care health care facilities (Bureau of Health Administration & Ministry of Public Health, 2012) and have 30 to 90 beds. They provide inpatient care, outpatient care, emergency services, operating rooms, labor rooms, and collaborate with primary care level services (Administration System Development Office, 2010). Nurse managers in community hospitals have broader roles than those in the other level hospitals, and they have to coordinate with both multidisciplinary teams and the community, handle a wide variety of roles with limited resources, and have broad knowledge to cope with day to day activities in their hospitals using creativity and resourcefulness (Paliadelis, 2005).
The Thailand Nursing and Midwifery Council (2013) broadly identified five competency domains for nurse managers which are: 1) leadership, 2) management and quality improvement, 3) communication and relationships, 4) awareness of codes of professional conduct, ethical, and legal practices, and 5) the policy and healthcare environment. Nurse mangers in Thailand who are members of this organization are expected to apply the five competency domains within their workplace context. Therefore, this study applied this framework to investigate the perspective of nurse managers and directors of nursing services in community hospitals.
In Thailand community hospitals, most head nurses are selected by higher executives for reasons other than having specified qualifications with the necessary skills and knowledge (The Policy and Planning of the Secretariat of Thailand Nursing and Midwifery Council, 2011). They often start as nurse managers, who are responsible for the quality of patient care delivered on their unit. Community hospitals service a large group of the Thai people who do not live in large cities. If nurse managers are not educated for the positions, the quality of patients’ overall care will be compromised, which leads to concern about whether Thailand can meet its health care goals. Several studies in Thailand have examined the competencies of nurse managers in general, regional, and university hospitals, but none specifically focused on nurse managers in community hospitals (Bureau of Nursing, 2005). In light of this concern, the purpose of this study was to investigate the competencies of nurse managers in the context of community hospitals from the perspective of nurse managers and directors of nursing services who work in community hospitals.
Methods
The qualitative descriptive design was implemented to explore the viewpoints of nurse managers in a community hospital about knowledge, skills, and personal characteristics from the perspective of nurse managers and directors of nursing services in community hospitals.
Sample and Setting
One district from each of 4 parts of Thailand was selected in the first sampling stage. Simple random sampling was used to select one community hospital as is recommended by Waltz et al. (2005). For the focus group, simple random sampling was used to select one community hospital from all hospitals in Thailand. The data were collected from 4 directors of nursing services and 6 nurse managers who worked in one of several community hospitals. One director of nursing services and five nurse managers from the same hospital were included in a focus group discussion. Three directors of nursing services and one nurse manager from different hospitals across the country were interviewed separately. The participants for interviews’ ages ranged from 48 to 55 years (M= 50.3, SD = 3.3). All of them had earned master’s degrees. The length of their experiences as nurse managers ranged from 2 to 12 years (M= 6.5, SD = 4.2). The ages of the focus group participants ranged from 38 to 55 years (M= 46.7, SD = 5.5). All of them had earned a bachelor’s degree and had experience working as a nurse manager from 6 to 13 years (M= 8.5, SD = 2.2). Most (83.3%) were nurse managers and 16.7% were directors of nursing service.
Data Collection Procedures
After approval from the Research Ethics Review Committee of the Faculty of Nursing Chiang Mai University, the researcher contacted the directors of nursing services at the selected hospital for permission to collect data. Then, the researcher individually contacted the four directors of nursing services and six nurse managers to sign an informed consent form and made an appointment for an interview or for participation in a focus group. The participants were asked for their permission to record the dialogue from the interview or focus group discussion on audiotape; the audiotapes were destroyed immediately after finishing the study. The researcher interviewed each of the three directors of nursing services and one nurse manager using the Interview Guide.
The Interview Guide was a semi-structured interview format consisting of three open-ended questions that asked them to describe and identify the essential competencies for nurse managers in community hospitals as well as to identify behaviors for each competency. Three nursing faculty members who were experts in qualitative methods reviewed the guide for strengths and weaknesses and provided feedback used to improve the guide.
Each interview took one to one and a half hours. Two focus group sessions were held, which lasted from 50 to 90 minutes. During the focus groups, the trained research assistants took notes on as much as possible, including the discussion and observations of nonverbal communication.
Data Analysis Procedures
The audiotapes from individual interviews and focus group discussions were transcribed. The interview data were analyzed using content analysis. The concept clarification of terms was done using the framework of competency for nurse managers of the Thailand Nursing and Midwifery Council defined as five domains: leadership, management and quality improvement, communication and relationships, awareness of codes of professional conduct, ethical and legal practices, and policy and healthcare environment (TNMC, 2013). The researcher repeatedly read the transcriptions, developed a categorization matrix, and coded the data within the categories by frequency, order, or intensity of the occurrence of words, phrases, or sentences (Elo & Kyngäs, 2008). Then, the words or sentences with the highest frequency were selected. The data were validated by the directors of nursing services and nurse managers who were interviewed or in the focus group. The researcher asked participants to support their statements with examples, and probed their answers for more information. The data were analyzed and interpreted by the researcher and the faculty advisers. If two significantly different data interpretations occurred, the data were discussed until we reached a consensus, as well as confirming the data using the field notes.
Results
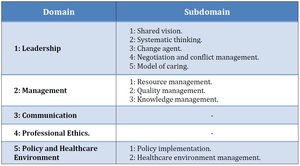
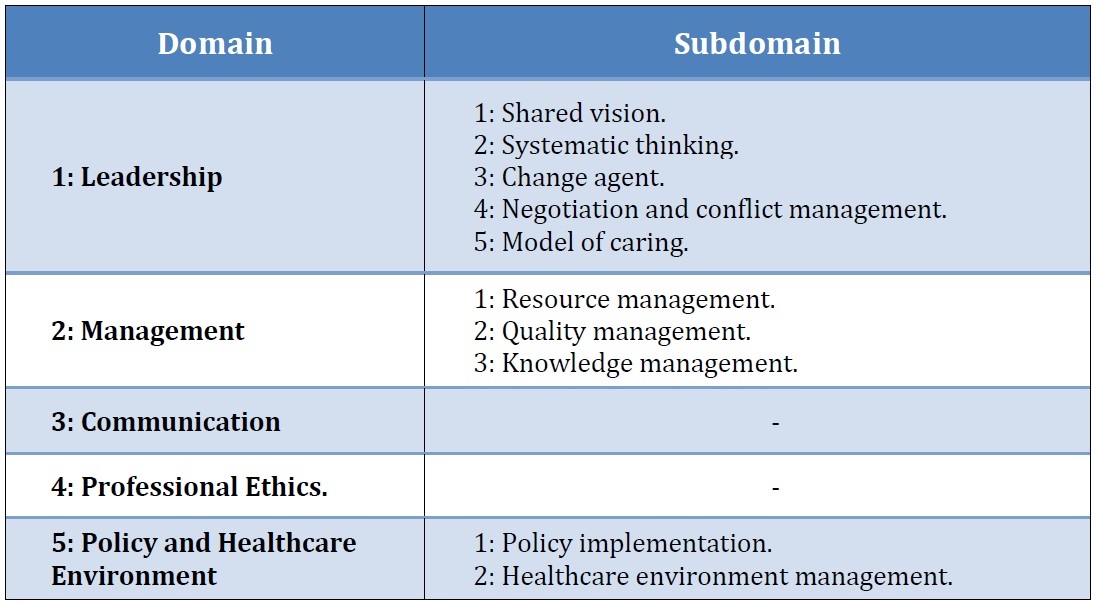
The five competencies for head nurses in community hospitals which were found in this study included leadership, management, communication, professional ethics, and policy and healthcare environment as summarized in Table 1.
It should be noted that they are the same as the Thailand Nursing and Midwifery Council domains. However, the subdomains found in this study were different from the Thailand Nursing and Midwifery Council: model of caring, sharing vision, and systemic thinking. These showed that context affected the different competencies. Each of these competencies is something all nurse managers should have been educated about before assuming the nurse manager position.
The five domains and their subdomains were summarized in the following section.
Domain 1: Leadership
Most participants defined leadership competency as
- “a team leader who thinks with a systemic perspective for goal achievement. A nurse manager must be a leader in the community and coordinate with the healthcare network and other organizations. They should practice good nursing care as a model of caring.”
The participants proposed that leadership is concerned with a shared vision, systemic thinking, being a change agent, negotiation, and a model of caring. Two participants stated,
-
“the nurse managers as leaders have to regulate goals, visions, and systematic procedures and negotiations to be an change agent and consultant to nursing subordinates.”
-
“Nurse managers need to use knowledge, skills, and abilities to motivate and lead other people to participate in and share their vision of the work.”
Subdomain 1: Shared vision.
For nurse managers to actually help achieve goals in their organization, they should have knowledge, experience, and characteristics to help them view the organization widely as a whole, and set a vision for the future. Participants state,
- “in achievement of the work … they have to set and share the vision for the future, and plan for both the short and long term continuously.”
Subdomain 2: Systematic thinking.
Nurse managers or leaders need to use information to create good decision-making and problem solving so that clients, providers, and the organization receive the overall benefits. Some participants described,
-
“To understand the issue and problem, each situation and problem should be classified in a step-by-step manner.”
-
“To understand the issue and problem, each situation and problem should be classified in a step-by-step manner.”
Subdomain 3: Change agent.
Nurse managers should be leaders of change and energize team efforts to participate in the desired changes. As most participants said,
- “nurse managers must be leaders in managing the process of change. …they have to plan and make efforts for subordinates to participate in the desired changes, especially in the clients’ care.”
One participant said that nurse managers need to provide the healthcare team with the data or other information for them to choose the best option when changes are needed. They need to :
- “Explain the information to subordinates who are faced with the change events until they accept them.”
Subdomain 4: Negotiation and conflict management.
The participants mentioned that nurse managers need to have strategies for giving in on some points and standing firm on others to satisfy both sides.
- “Leaders should negotiate and manage the conflict through using the information and reasons for giving some points and standing firm. Both providers and clients can see that the result is satisfactory on both sides.”
Some participants said that the nurse managers often work with staff who have disagreements. One participant agreed with them and recommended that nurse managers should manage a dispute through sharing the needs of each group for agreement consensus.
- “I think if nurse managers are competent, they can work with the team members who disagree about something to help them reach a consensus.”
Subdomain 5: Model of caring.
Nurse managers, as leaders, need to be experts in nursing care and consultants in nursing for the team, as well as good role models of caring. Some participants stated,
-
“Collecting knowledge and experience in management and facilitating the team for caring in a unit and community has to be demonstrated in the nurse manager position and model of nursing care.”
-
“The expertise of leaders must show broad knowledge of nursing service in community hospitals. They ought to be the consultants in the nursing care team when their subordinates are faced with a difficult situation.”
Domain 2: Management
Management is an essential competency. The participants mentioned that to be competent in management, nurse managers should manage resources, quality care, and nursing knowledge in the unit and in the community. Participants stated,
- “Competent nurse managers in management need to be educated for management …that resource management, which includes both human resources and supplies in the unit and community, and covers the quality of nursing management.”
Subdomain 1: Resource management.
Resource management is involved in human, supplies, instruments, and budgets. Participants defined resource management as
- “…that nurse managers can manage human resources, plan the appropriate workforce including the development of career paths, retain staff, and assess performance. For budget management, nurse managers have to plan the budgets for long-range planning and estimate funding needed to meet the organization’s objectives. For supplies management, they should prepare and forecast sufficiently for the month.”
Some participants mentioned and focused on the effective cost of resources in a unit and the community.
- “Resource management competency…the human resources, budget, and supplies are used effectively cost-wise both in the unit and community.”
Subdomain 2: Quality management.
All participants described how nurse managers must be leaders in quality management, collaborating with subordinates and the healthcare team in the unit and the community through activities related to establishing, maintaining, and assuring high quality care, and setting the standards and process of evaluating and monitoring the quality of care given in a unit and community.
- “… Nurse managers lead the subordinates to assure and improve the quality of service. Setting goals and standards are discussed by brainstorming. Data collection for interpretation is essential for implementation improvement. Monitoring nursing care should use several methods.”
Some participants suggested nurse managers should collaborate with the healthcare team to analyze and plan the expected outcome results to the standards and process of outcome management.
- “Nurse managers should integrate the standards to practice in a unit and community.”
Subdomain 3: Knowledge management.
For quality care, information is important to meet the goals of care. Participants recommended nurse managers should have the ability to organize, collect, share, and analyze the information about nursing care effectively, and to be a facilitator and consultant with subordinates, networks, and the community. Some participants suggested nurse managers also facilitate subordinates’ knowledge management and share information with healthcare teams and other organizations.
- “I suggested that nurse managers should be the supervisor in the process of knowledge management in a unit and the community to share their knowledge and problems with each other.”
Domain 3: Communication
Communication is a competency expected for nurse managers. Participants said that nurse managers should establish relationships in order to have the ability to transfer information and understanding from one person to another by both verbal and nonverbal communication and be able to use technologies to access the available information and to communicate nursing knowledge effectively.
-
“They should establish relationships and trust, and use the technologies in investigation and communication effectively.”
-
“Nurse managers ought to have a relationship with other people in the unit, other organizations and other disciplines. They should communicate both verbally and nonverbally as well as use technology for quality service.”
One participant described how effective communication is based on the skills and strategy of nurse managers, because they need to transfer the information and understanding from one person to another.
Domain 4: Professional Ethics.
The participants said that nurse managers should behave in a normal way and have knowledge about ethics, law, and patient rights.
- “Nurse managers engage in law, ethics, and professional conduct in their roles. They must work with honesty and justice.”
Some participants stated that nurse managers must facilitate subordinates’ ability to advocate for recipients of healthcare, human and patient rights, and understand to how to advocate for patient and provider rights. Most participants warned nurse mangers about monitoring of human rights.
- “All patients must be informed of their rights, and nurse managers should advocate for providers’ and patients’ rights.”
Domain 5: Policy and Healthcare Environment.
Participants described the behaviors of nurse managers needed in this domain, which were categorized separately with two subdomains: policy implementation and healthcare environment management.
Subdomain 1: Policy implementation.
Participants described policy implementation as transferring policies to subordinates and moving the unit toward its goals by assigning activities for members to perform. They should have the ability to prevent and control the determinants that may cause the problems that can be forecasted in the unit and the community.
- “Participating in policy regulation of subordinates in the unit is essential. Nurse managers have to transfer related policies to subordinates. One leg steps on the community and the other steps on the unit.”
Some participants stated,
- “Nurse managers have to move the unit toward their purpose or goals by assigning activities that the organization or members perform. They need the ability to forecast the impacts of diseases, and then prepare to prevent and control the determinants to decrease problems.”
Subdomain 2: Healthcare environment management.
Participants said that every hospital now has to be a healthy workplace, which is consistent with the policy of the Ministry of Public Health. So, nurse managers need the ability to work with subordinates and facilitate the environment for a healthy workforce and a healthy environment. Most participants said that nurse managers are required to effectively plan, implement, control, and evaluate the healthcare environment for the patient and healthcare team for safety and health. They should facilitate having sufficient supplies for safety and a healthy environment.
-
“Standards of a healthy workplace are required for nurse managers so they can manage the environment for patient and provider safety.”
-
“Nurse managers need to have the proficiency to plan, implement, control, and evaluate the healthcare environment, and they should sufficiently facilitate the supplies for the safety and health of clients and providers.”
Discussion and Implications
The Thailand Nursing and Midwifery Council recommended that nurse managers’ competencies should be evaluated by the hospitals, and they should be required to complete an educational program before being promoted into their positions (TNMC, 2013). However, most nurse managers were not selected for their positions based on these criteria (The Policy and Planning of the Secretariat of Thailand Nursing and Midwifery Council, 2011). One finding of this study was that most participants thought they were not prepared for their positions.
The content analysis supported the five domains of the Thailand Nursing and Midwifery Council: leadership, management, communication, professional ethics, and policy and healthcare environment. Leadership and management competency are consistent with Chase (2010), who studied nurse manager competency, which revealed that human skills, leadership skills, and financial management are the essentials competencies for nurse managers. In many studies, researchers found that the competencies nurse managers need to ensure quality care and administration include leadership, financial, management or organization, communication, human resource, collaboration and team, clinical skills and knowledge, relationship, thinking, integrity and awareness of regulatory requirements, informatics and technology, and conflict resolution (Balke & et al, 2006; Harrison, 2005; Jeans & Rowat, 2004; McCarthy & Fitzpatrick, 2009; Russell & Scoble, 2003).
Participants wanted nurse managers in community hospitals in Thailand to be experts in nursing care, which would make them competent in a model of caring. Technical skills are essential for nurse managers (Chase, 2010). Participants suggested that not only do nurse managers have to manage and practice in units but in the community also. This standard of competency and cooperation in the community differs from the standards of the Thailand Nursing and Midwifery Council that did not specifically study community hospitals, because the context and innovative technologies make the capability of healthcare services different in each country and each level hospital (Boyle, 2011). Eldridge and Judkins stated that competency of nurse managers should be based on the integration of need-based community services and cross-disciplinary management for success in administration (Eldridge & Judkins, 2003).
The Thailand Nursing and Midwifery Council (2013) and Promsorn (2007) studied competencies for nurse managers in a Thai context and concluded that moral principles and ethics, and a code of professional conduct, ethics, and law were important competencies for nurse managers. In this study, it was found that professional ethics are essential competencies for nurse managers in community hospitals. But most studies in other countries did not mention this. Moreover, there are some competencies such as communication and policy and healthcare environment that were not included (Eldridge & Judkins, 2003).
Competencies for nurse managers in each health service level are different depending on their context (Bureau of Health Administration & Ministry of Public Health, 2012). Thai healthcare policy focused on the participation between government and community, the health care environment, strong community, holistic integration, and human-centered care (Faramnuayphol et al., 2011). So, nurse managers in community hospitals have to cooperate with the community. Competencies can be encouraged or trained if not sufficient (Duffield, 1992). Educational programs could offer mastery programs or other organizational leadership programs. The results of this study can be used for assessment and to be guidelines for curriculum construction. The Thailand Nursing and Midwifery Council studied core competencies for all nurse managers in Thailand. Nurse managers should be prepared before stepping into their positions and have a qualified education, at least at the master’s degree level, which contributes to the development of the required attitudes, knowledge, and skills. Also, these competencies should be integrated in the administration program.
Moreover, this finding focused on nurse managers in the community hospitals and is based on the opinions of public nurse executives. So, some of the findings differ from the concept of the Thailand Nursing and Midwifery Council. It fits with the context of community hospitals.
Limitations and Strengths
The number of participants for the interviews and the number of participants in the focus group was limited. A purposive sampling technique was used in this study, and participants were included based on their willingness to participate in the study. However, the intent of the qualitative method is to probe a detailed perspective of a small number of persons (Waltz et al., 2005). Choosing to use the Thailand Nursing and Midwifery Council framework might have presented a different domain from being identified. However, the goal in this study was to use the framework to see if it matched the interviewees’ perspectives.
The nurse managers who participated in this study came from four regions in Thailand, and they represented each region of the country. Future research should extend to the competency for nurse managers in other levels of hospitals, and with a representative sample.
Conclusion
The domains and subdomains revealed in this study are essential for nurse managers in community hospitals in Thailand. The essential competencies include five domains: leadership, management, communication, professional ethics, and policy and healthcare environment, as identified by the Thailand Nursing and Midwifery Council. However, some characteristics in each domain and subdomain are different from the Thailand Nursing and Midwifery Council. From the study, not only do nurse managers in community hospitals need to practice management, but they also need to do so in nursing care. In addition, nurse managers have to manage both the clinical unit and the community or network. It is very important that they are adequately educated to fulfill their roles.
Biographical Notes
Kanjananat Tongmuangtunyatep, PhD, RN, is affiliated with Boromarajonani College of Nursing, Chainat.
She can be reached at Boromarajonani College of Nursing, Chainat, 248 Chainat District, Chainat Province, 60000 or by e-mail at tomtam2512@gmail.com.
Marry Lynn, PhD, RN, is a professor and Assistant Director, Quality and Training, UNC-CH Office of Human Research Ethics, Department of Nursing, School of Nursing, the University of North Carolina at Chapel Hill.
She can be reached at The University of North Carolina at Chapel Hill, School of Nursing, Carrington Hall, CB #7460, Chapel Hill, NC 27599-7460.
Wipada Kunaviktikul, PhD, RN, is a professor and Dean of the Faculty of Nursing, Chiang Mai University, Chiang Mai province, Thailand.
She can be reached at the faculty of Nursing, 110/406 Inthawaroros road, SriPhum, ChiangMai 50200.
Acknowledgements
1
Correspondence concerning to this paper should be addressed to Dr.Kanjananat Tongmuangtunyatep at Boromarajonani College of Nursing, Chainat, 248 Chainat District, Chainat Province, 17000 and E-mail: tomtam2512@gmail.com
The authors would like to express gratitude to the Thailand Nursing and Midwifery Council for a partial funding support of this study. Importantly, deep thanks are given to experts contributing and the participants in this study